Build Your Mental Gym Part 3 of 13: Holistic Regulation Protocol for Fight-Flight State
Introduction to this Series:
Build Your Mental Gym: A Brain Health Protocol for Women in Tech (in 13 parts)
You’re ambitious, driven, and focused. You’re constantly climbing, always pushing yourself, and you’ve learned to navigate a world that demands relentless hustle. But lately, things aren’t adding up the way they should. You’re “wired but tired,” struggling with the fog, fatigue, and hormonal chaos. No matter how much you optimise, there’s a nagging sens…
What To Expect: You know that feeling when your mind won’t stop spinning, your chest feels tight, your heart’s racing, and even the smallest task feels like a mountain? When you’re answering emails with one eye twitching, holding your breath between meetings, and somehow still feeling behind? That’s not just “being busy.” That’s your fight-or-flight response, your body stuck in survival mode.
When this state becomes the norm, not the exception, it starts to erode your focus, drain your energy, and distort your sense of what’s urgent versus what’s actually important. It doesn't happen all at once. It’s subtle. You might call it “just a rough week,” until those weeks stack up and you realise you don’t remember the last time you felt truly rested, creative, or in control.
In this part of the series, I’ll walk you through the exact tools that help people interrupt this cycle using science-backed biohacks that take into account female physiology. Not vague advice or lofty affirmations, but real, science-backed techniques that work with your biology. You’ll learn how to use your breath to signal safety to your body. How to move in ways that restore rather than deplete. And how to ground your mind without needing to retreat from the world or your ambition. This isn’t about checking out. It’s about building a body and brain that can stay checked in, without burning out.
Fight or Flight (Hypo-Vigilance /Arousal)
When you enter this state—often marked by lowered arousal or vigilance—you may unconsciously disconnect from your physical self in an attempt to feel safe. The body’s way of coping becomes quiet: seeking distraction, creating distance from your sensations, subtly withdrawing from the moment. Rather than identifying internal triggers, you might externalise your discomfort, attributing thoughts and emotions to your environment or others.
Coping can look like scrolling social media without really seeing it, disappearing into a TV show, or getting lost in fantasy or daydreams. These aren’t flaws, they’re adaptive strategies your nervous system has learned to help you survive when the world feels too much. But over time, these patterns can create a feedback loop of avoidance, leading to social withdrawal, emotional numbness, and symptoms that mirror depression.
It’s important to understand that the fight-or-flight response doesn’t always come with an obvious escape route. Modern life doesn’t always let you slam the brakes. Some stressors—deadlines, caregiving, chronic health conditions—don’t just go away. Even when you seek out support or connection, your system may still be activated, wired with the physiological alertness of threat.
This is why nervous system work begins with awareness. Recognising that your responses may be shaped by your environment—but not wholly defined by it—is a radical act of reclamation. Your responsibility is not to control every trigger. It’s to learn your patterns and responses with compassion and curiosity, so you can slowly begin to choose differently. Not from a place of blame, but from a place of ownership.
The Unique Female Experience:
While this concept doesn’t yet have broad scientific consensus, an intriguing line of research suggests that the classic "fight-or-flight" response may manifest differently in women, often along the lines of what some researchers term tend-and-befriend.
Tending refers to nurturing behaviours that aim to protect the self and others—particularly their offspring—in times of stress. This pattern appears to be influenced by the hormone oxytocin, which promotes a sense of safety and reduces distress. In situations of perceived threat, elevated oxytocin levels have been observed to encourage caring behaviours and social engagement, potentially dampening the traditional fight-or-flight response.
Often associated with childbirth and breastfeeding, oxytocin also plays a central role in affiliative behaviours rooted in our instinctive need for connection. Emerging evidence also indicates that during positive social interactions, oxytocin may interact with the body’s opioid system, which governs responses to pain and reward. This interplay is thought to help modulate stress responses, though formal studies remain limited and inconclusive.
The “befriend” part of the response refers to strengthening and relying on social networks during times of stress. The proposed mechanism underlying this pattern draws from the attachment-caregiving system, a set of behaviours and hormonal responses thought to promote bonding and mutual support.
Neuroendocrine research across animal and human models suggests that oxytocin, alongside female reproductive hormones and endogenous opioid peptides, may be central to this process. Still, this area of study is nascent and not without its critiques.
💡 While promising, these findings remain speculative and under-researched. Over-attributing such behaviours to caregiving instincts risks reinforcing gender stereotypes. That said, this theory offers an important insight: as women, our stress responses may not always fit the standard models we've been taught. Recognising these differences can help us make sense of our instincts and honour them. I want to be mindful of any blanket recommendations, but it is my duty to share the latest research with you.
Some examples of behavioural responses of this theory in action, as per the study:
This theory suggests that when women are under stress, they often respond by caring for others or seeking connection. It’s the classic “tend and befriend” pattern, and it lines up with how social most of us naturally are. What’s still unclear is whether this is a learned behaviour or something wired into our biology. Probably a bit of both.
Interestingly, this tracks with what we now know about community and health. In Blue Zones — the regions where people consistently live past 100 — community involvement (often faith-based) plays a big role. And the WHO now classifies loneliness as a global health issue, the risks of which are a 50% increase in dementia, and a 30% jump in heart disease or stroke. The numbers are alarming, but the takeaway is simple: connection matters.

Art by Sophie Blackall from Things to Look Forward to Across species, females tend to lean into nurturing and bonding under stress, while males are more likely to act out or shut down. Some researchers believe this developed as a protective strategy for women and children. That said, just because we see these behaviours more in women doesn’t mean men aren’t capable of them. It might just be that society gives women more permission to express themselves.
Now, here’s where nuance is important. Seeking support doesn’t always lead to safety. Because tending and befriending is a stress response, it can also keep people stuck, for example, staying in an unhealthy relationship because the urge to connect and calm feels stronger than the impulse to run. That’s not weakness. That’s biology doing its thing even when the situation doesn’t serve you.
These patterns aren’t one-size-fits-all. They’re shaped by your attachment style, past trauma, coping mechanisms, and the whole nervous system story. And while this theory isn’t yet gospel in the scientific world, it does remind us of something important: women’s stress responses might look different, and that doesn’t make them less valid. It just means the old models were incomplete.
Physical Signals You Should Monitor:
Your body speaks volumes before your mind catches up. These are the signals it sends when you’re under stress, not to scare you, but to help you pay attention. Think of this as a dashboard of early indicators. Your goal should be to learn to read them before they become red flags.
🧠 Track Using Interoception (no wearable or test needed)
Interoception is your brain’s ability to sense and interpret internal signals from your body, like heart rate, hunger, temperature, or breath. It’s how you detect what’s happening inside you, often before you’re consciously aware of it.
Pupil Size
What to monitor: Notice if your pupils feel overly dilated or if you’re unusually sensitive to light. This often shows up as visual strain or slight tension around the eyes.
Why it happens: In a stress state, your pupils dilate to widen your field of vision and increase your awareness of threats.
Why it matters: Constant dilation can strain your eyes and contribute to headaches, visual discomfort, and even sleep disturbances (as your body struggles to wind down).
How to use the signal: If you’re squinting more than usual, avoiding sunlight, or rubbing your eyes constantly, it’s a sign your nervous system is stuck in alert mode. Take that as your cue to ground yourself: try breathwork, dim the lights, or go screen-free for an hour.
Digestion
What to monitor: Look for patterns of bloating, constipation, loose stools, or loss of appetite when you're under pressure.
Why it happens: Blood is redirected away from the digestive system during stress. Your body deprioritises digestion to focus on survival.
Why it matters: Chronically impaired digestion affects nutrient absorption, energy production, and gut health which in turn messes with mood and immunity.
How to use the signal: If your digestion consistently worsens during periods of stress, that’s data. You don’t need a supplement, you need nervous system down-regulation. Slow meals, deep breaths before eating, and gentle movement post-meal go a long way.
Salivation
What to monitor: A dry mouth, especially when you’re not dehydrated.
Why it happens: Saliva production slows in fight-or-flight because digestion is not prioritised.
Why it matters: Low salivation increases risk for tooth decay, oral infections, and digestive issues (saliva contains key enzymes for breaking down food).
How to use the signal: If your mouth often feels dry during the day, it’s a subtle but powerful clue that your stress response is too activated. Use that moment to do a reset with a quick nervous system practice or hydration break.
Relational Ability
What to monitor: Are you feeling emotionally unavailable, defensive, or just too drained to connect?
Why it happens: In survival mode, your brain downshifts from complex social reasoning into basic protection.
Why it matters: Disconnection, when chronic, is a compounding stressor. It erodes support systems, creates loneliness, and can mimic depression.
How to use the signal: Instead of powering through social fatigue or retreating into isolation, acknowledge it. Try nervous system regulation first, then return to connection. Don’t force relational depth when you’re dysregulated.
⌚ Use a Wearable
Resting Heart Rate (RHR)
Note: RHR is different from HR. RHR (Resting Heart Rate) is your heart rate when you're completely at restIt’s a stable baseline indicator of overall cardiovascular health and stress load. HR (Heart Rate) refers to your heart rate at any given moment. It fluctuates constantly based on activity, emotions, posture, hydration, and more. Think of RHR as the signal you track over time to assess recovery and chronic stress, while HR is the moment-to-moment metric that can tell you how your body is responding right now.What to monitor: Your resting heart rate ideally tracked over time, not just as a one-off. Your wearable will give you a baseline over a few days of use.
Why it happens: Under any form of stress (including alcohol, sex, dancing, and more, by the way!), your sympathetic nervous system kicks in, making your heart beat faster to deliver more blood to muscles and vital organs.
Why it matters: A consistently elevated resting heart rate, without adequate recovery, is often a sign of chronic stress. Over time, it increases cardiovascular strain, messes with your energy levels, and impacts recovery.
How to use the signal: If your heart rate is creeping up over days or weeks (even by 5–10 bpm), treat it as an early warning sign. Build in more recovery, not more workouts, not more coffee, not more pushing through.
💡 Benchmark ranges (female):
• Age 26–35: 42–68 bpm
• Age 36–45: 45–69 bpm
You're aiming for the lower-middle end of that range if you’re healthy and not overtraining.
Blood Pressure
What to monitor: Trends in your systolic and diastolic readings throughout the day (morning and evening).
Why it happens: Stress causes blood vessels to constrict, raising blood pressure to push oxygen-rich blood toward vital organs and muscles.
Why it matters: Prolonged elevation raises your risk of hypertension, stroke, and cardiovascular disease, even if you feel "fine."
How to use the signal: If you’re noticing upward trends, especially during high-stress weeks, treat it as a signal to intervene early with regulation practices, salt intake moderation, and better sleep.
💡 Healthy range: Below 120/80 mmHg for most adults. Monitor for consistent spikes, not just isolated readings.
Oxygen Circulation to Vital Organs
What to monitor: Your breathing rate and depth, especially if you’re breathing shallowly or feel short of breath without exertion.
Why it happens: The body hyper-oxygenates under stress to stay sharp and reactive.
Why it matters: Chronic overbreathing can reduce CO₂ tolerance, disrupt blood ph, and create symptoms like dizziness, fatigue, and anxiety.
How to use the signal: Focus on breathing practices that train CO₂ tolerance (like box breathing or extended exhale). If you’re always mouth breathing or sighing, that’s a red flag.
🧪 Get a Test
Fuel Availability (Blood Glucose Levels)
What to monitor: Fasting glucose and glucose variability throughout the day.
Why it happens: During stress, the liver dumps glucose into the blood for immediate energy.
Why it matters: Chronic spikes can drive insulin resistance, metabolic dysfunction, and hormonal imbalances — even in people who eat “clean.”
How to use the signal: If you have access to a CGM or periodic bloodwork, use it to track glucose spikes during periods of emotional or work stress, not just after meals.
Adrenaline (Epinephrine)
What to monitor: Not directly testable at home, but blood panels or 24-hr urine catecholamine tests can give insight.
Why it happens: Adrenal glands flood the body with adrenaline in response to perceived threat.
Why it matters: Chronically high levels can disrupt sleep, create cardiac rhythm issues, and lead to adrenal dysregulation.
How to use the signal: If your panel shows consistently elevated catecholamines, that’s a sign to aggressively prioritise regulation, sleep hygiene, and slow, restorative movement.
Blood Clotting
What to monitor: Coagulation markers like D-dimer or platelet aggregation (requires lab testing).
Why it happens: The body prepares for injury during stress by enhancing clotting.
Why it matters: Chronic overactivation can raise your risk of clotting disorders like DVT, pulmonary embolism, or stroke.
How to use the signal: If you’re at risk or have signs of poor circulation, speak to your doctor about testing. Lifestyle stress is part of the picture, not just genetics.
Dilation of Bronchi
What to monitor: Lung function tests like spirometry, or subjective symptoms like breathlessness or chest tightness.
Why it happens: Bronchi expand to take in more oxygen when under pressure.
Why it matters: Chronic dilation or inflammation worsens respiratory conditions like asthma and impairs performance.
How to use the signal: If you’re wheezing, out of breath during basic tasks, or struggling with breath control, don’t brush it off. Look into nervous system regulation and potentially medical support.
Defensive Responses
What to monitor: Startle responses, physical tension, or feeling “on edge” all the time.
Why it happens: Your nervous system is trained to prepare you for conflict or escape.
Why it matters: Being stuck in this mode keeps cortisol high, impairs sleep, and impacts mood regulation.
How to use the signal: Learn to downshift your body with practices that mimic safety like weighted blankets, long exhales, or grounding movement.
Fuel Storage + Insulin Activity
What to monitor: Fasting insulin, HbA1c, and HOMA-IR (blood tests).
Why it happens: Stress inhibits insulin’s effectiveness to keep glucose available for action.
Why it matters: Insulin resistance doesn’t just lead to diabetes — it’s linked to inflammation, fertility issues, brain fog, and more.
How to use the signal: If blood sugar is stable but insulin is high, your body is working harder than it should. Fix the root: lower chronic stress, reduce visceral fat, increase muscle mass, and improve sleep.
Immune Response
What to monitor: White blood cell counts, chronic low-grade inflammation markers like CRP, and how often you’re falling sick.
Why it happens: The immune system takes a backseat during acute stress to conserve energy.
Why it matters: Suppression makes you more vulnerable to illness, slows recovery, and contributes to autoimmune conditions.
How to use the signal: If your immunity’s tanking during busy seasons, it’s not just the germs. Stress is lowering your defence. Sleep, nourishment, connection, and rest are non-negotiable here.
Why I’m Not Offering Behavioural Advice Here (Yet): I’m intentionally leaving this section open for now.
Yes, you can google “how to respond to stress” and find plenty of suggestions — but here’s the thing: most of those behavioural recommendations haven’t been studied on female bodies. They also rarely account for how social conditioning shapes our responses, especially for women. And they almost never consider neurodivergent patterns or how behaviours might look different for people outside the so-called “norm.”
Right now, I’d rather be honest about that gap than offer generic advice. I’ll update this section when (and if) I come across research that feels more rigorous, inclusive, and representative of real-world experiences.
The Protocol
When your body is stuck in fight-or-flight, you don’t need to push harder, you need to help it feel safe again. This protocol is designed to guide you out of that reactive state, one step at a time. Don’t rush it. Don’t stack everything. Start with one, and build from there. The goal is progress and physiological trust, not perfection:
Step 1: Regulate your breath to signal safety
When your body is in a reactive state, your breath becomes shallow, fast, or erratic, a direct reflection of sympathetic nervous system dominance. One of the fastest ways to interrupt this and bring your system back into regulation is by using your breath to stimulate the vagus nerve. This tells your brain: we’re safe now. Start with any one of these techniques, whichever feels easiest to access in the moment.
Box Breathing: This simple but powerful technique helps regulate your resting heart rate and heart rate variability, two core indicators of how well your body is managing stress. By slowing your breath, you help activate the parasympathetic nervous system (aka rest-and-digest mode), which calms your body and mind.
How to do it:
Inhale through your nose for 4 seconds
Hold for 4 seconds
Exhale through your mouth for 4 seconds
Hold for 4 seconds
Repeat for 1–2 minutes. You can also try a 4–7–8 rhythm if that feels better.Alternate Nostril Breathing (Nadi Shodhana): This yogic breathing technique works on the autonomic nervous system by gently rebalancing both brain hemispheres and calming the body. It’s particularly helpful when you’re feeling overstimulated or need to reset after an intense day.
How to do it:
Step 1: Use your right thumb to close your right nostril
Step 2: Exhale slowly through your left nostril
Step 3: Inhale deeply through the left nostril
Step 4: Close your left nostril with your ring finger and exhale through the right
Step 5: Inhale through the right nostril
Repeat for 10 rounds or until your mind feels clearer and your body less tense.Perform the physiological sigh: This is a quick, science-backed technique used to calm the nervous system in real time. Just a few rounds can reduce anxiety and bring you back into your body, fast.
How to do it:
Take two sharp inhales through the nose — one full inhale, followed by a quick second sip of air at the top
Exhale fully through the mouth until your lungs are empty
Repeat 1–3 times
Step 2: Discharge stress through muscle tension and release
When your nervous system is stuck in overdrive, your muscles hold the score — often clenching without you even realising it. Progressive muscle tension and release helps reset this by doing the opposite: you deliberately tighten, then fully let go. This gives your body a physical cue that it’s safe to relax. It’s especially effective when you feel wired, restless, or like you can’t “drop” back into your body.
You only need 5–10 minutes, and you can do it seated, without any special setup.
How it works:
As you inhale, gently tense one muscle group for 4–10 seconds (don’t strain).
As you exhale, release that muscle group completely in one go.
Pause for 10–20 seconds before moving to the next group.
Here’s a sequence to follow — but feel free to adapt depending on what’s accessible or needed:
→ Face (forehead, around eyes and nose, cheeks, jaw)
Close your eyes and lips tightly. Frown deeply, clench your jaw, wrinkle your nose.
Exhale and let it all drop.
→ Shoulders, neck, upper back
Raise your shoulders to your ears. Press your chin gently to your chest.
Exhale and let your shoulders fall away from your ears.
→ Wrists, forearms, hands
Make a tight fist and curl your wrists inward.
Exhale and shake it out.
→ Chest and stomach
Curl forward slightly, engaging your abs and chest like you’re hugging in.
Exhale and release the fold.
→ Hips, glutes, upper thighs
Squeeze your glutes, press your thighs together, and hold.
Exhale and let the tension go.
→ Lower legs and feet
Flex your calves, curl your toes tightly toward the sole.
Exhale and soften your entire lower body.
Even one round of this can make your body feel quieter. If you’re short on time, just target the areas where you hold the most tension — shoulders, jaw, or stomach are usually good bets.
Step 3: Use cold therapy to signal safety
Cold exposure, done gently and intentionally, can help shift your body out of a fight-or-flight state by stimulating the vagus nerve and lowering sympathetic activation. It’s a physical way to tell your nervous system: you’re safe now. But it’s important to listen to your body: skip this if you’re pregnant or actively menstruating, since your system is already in a heightened state.
You’ve got two options here. Use whichever feels most accessible in the moment:
Option 1: Spot cooling with a cold compress
Apply a cold compress for 3–4 minutes at a time to areas where you feel stiffness or tension — shoulders, wrists, thighs, lower back. This helps reduce inflammation and muscle guarding.
✳️ Avoid using cold therapy on your neck or above.
Option 2: Ice water hand immersion
This one’s great for quickly calming a racing system.
Fill a large bowl with equal parts ice and water.
Submerge both hands for 10 seconds.
Remove them, then go back in for 30 seconds.
Take a 30-second break, then repeat.
Do up to 4–5 rounds, or until you feel a shift.
This sends strong calming signals via cold receptors in your hands, which are linked to thermoregulatory and autonomic pathways. In plain terms, it helps cool both your body and your stress response.
If you're feeling overwhelmed or fidgety, this method is fast, physical, and deeply regulating, like hitting the reset button.
Step 4 (optional): Activate your physical senses for sustained stress relief
This step is about harnessing the power of your senses to create a lasting feeling of calm. If you already have a Sensory Plan that works for you, now’s the time to use it. But if not, consider tapping into one or more of the following sensory experiences to help ground your nervous system and create a sense of safety:
SIGHT: Look at photos of loved ones or tranquil nature scenes. Let yourself fully absorb the calm and positive feelings they bring, even for just a few moments.
SMELL: Aromas can be incredibly calming. Light a candle, diffuse some essential oils, or burn incense with soothing scents like lavender, rosemary, or jasmine. These smells can directly influence your limbic system, which helps regulate emotions.
TOUCH: Engage with something tactile. Wrap yourself in a soft blanket, feel the earth under your bare feet, or indulge in a warm bath. This tactile grounding helps anchor you back into your body and out of the fight-or-flight zone.
TASTE: Sip on a calming herbal tea — think chamomile or lavender — or enjoy a soothing herbal candy. Take your time to really taste and savour each bite or sip. This act of mindful consumption can activate the parasympathetic nervous system and help you unwind.
SOUND: Play calming music, or sit quietly and listen to natural sounds, like wind rustling leaves or birds chirping. Let the soothing rhythms reset your mental state, guiding you into deeper relaxation.
MOVEMENT: Sometimes, a gentle rhythm is all you need. Go for a walk, bike ride, or swim, or even try something slower like knitting. Focus on the sensations of movement and how they help release tension and ground you in the present.
These are simple, accessible ways to bring your body and mind into a calm, grounded space, helping to mitigate stress long-term. You don’t need to do them all at once. Just experiment with the ones that resonate with you most.
Step 5: Reach out to a trusted friend, loved one, or licensed medical expert for support
When you're starting to feel better, it can be incredibly helpful to lean on others for emotional or practical support. This step is about acknowledging that you're not in this alone and that support from a friend, family member, or professional can make a world of difference. Whether it's just someone to talk to or a trusted expert who can offer more tailored guidance, connecting with someone who understands your experience can be a key part of the recovery process.
Step 6: Continue practising the general protocol recommendations in this chapter as you begin to feel better
Once you start feeling more grounded and balanced, continue to practice the protocol steps outlined in this chapter. These steps are not quick fixes. They’re tools that can be integrated into your routine to maintain long-term resilience. Regularly using these techniques will help you manage stress, stay calm under pressure, and keep your body and mind in a more regulated state, so you’re better prepared when challenges arise.
Step 7 (Optional): Support Your Body Based on Your Menstrual Phase
Your body’s needs shift across your cycle. Whether you’re bleeding, ovulating, or somewhere in between, small, phase-specific adjustments to how you eat, move, and rest can make a big difference in how resilient you feel.
You can use your period tracking app to identify which phase you're in and follow the suggestions below to support your physical and hormonal recovery as you regulate your nervous system.
→ Menstruation Phase
Prioritise additional sleep: It’s common to feel more physically depleted during this time. Let yourself rest without guilt. Your body is doing a lot behind the scenes.
Light exercise: Gentle movement is more helpful than intense workouts here. Think: walking, stretching, or restorative yoga.
Heat therapy: Use a warm compress or bath to soothe cramps and relax your muscles.
Blood sugar awareness: If you're getting intense mood swings or cravings, a continuous glucose monitor (CGM) analysis can help you pinpoint patterns that may be spiking hormones and affecting energy.
Smart fuelling: Opt for iron-rich and warming foods like soups, dark leafy greens, legumes, and high-quality protein. Keep processed sugar low to prevent blood sugar rollercoasters.
Skip aggressive fasting: Calorie-restrictive fasts during menstruation may raise inflammation and worsen recovery. If fasting is part of your lifestyle, check in with a medical expert.
Supplementation (if needed): Nutrients like vitamin C, iron, magnesium, zinc, and omega-3s can support pain management and recovery. Personalise dosages with professional support.
→ Follicular Phase
Managing low energy: Early in this phase, estrogen is rising but still low. You may feel sluggish. Stick with good sleep habits and experiment with the rest strategies outlined earlier in the course.
→ Ovulation Phase
Ovarian pain or acne: These symptoms can be signs your body is struggling to clear excess estrogen. Increase your intake of cruciferous veggies and fibre to support detoxification and gut motility.
Zinc support: Zinc is crucial for ovulation, yet natural levels are at their lowest. Add zinc-rich foods like pumpkin seeds and nuts and consult a practitioner if considering supplements.
→ Luteal Phase
Cravings and calorie needs: Your metabolism ramps up during this phase. Don’t ignore hunger. Eating enough (especially protein, healthy fats, and fibre), even if you’re on a diet, stabilises blood sugar and helps ease PMS.
Pain support: Magnesium-rich foods (leafy greens, seeds, nuts, dark chocolate) can calm your nervous system and reduce physical tension.
Bloating, brain fog, PMS: Hydration is key. Stick to water or herbal infusions. Limit caffeine and sweetened drinks, which can dehydrate and spike heart rate.
Supplementation (if needed): Omega-3s can ease both mental and physical PMS symptoms. Consider flaxseeds, walnuts, or a high-quality supplement under professional guidance.
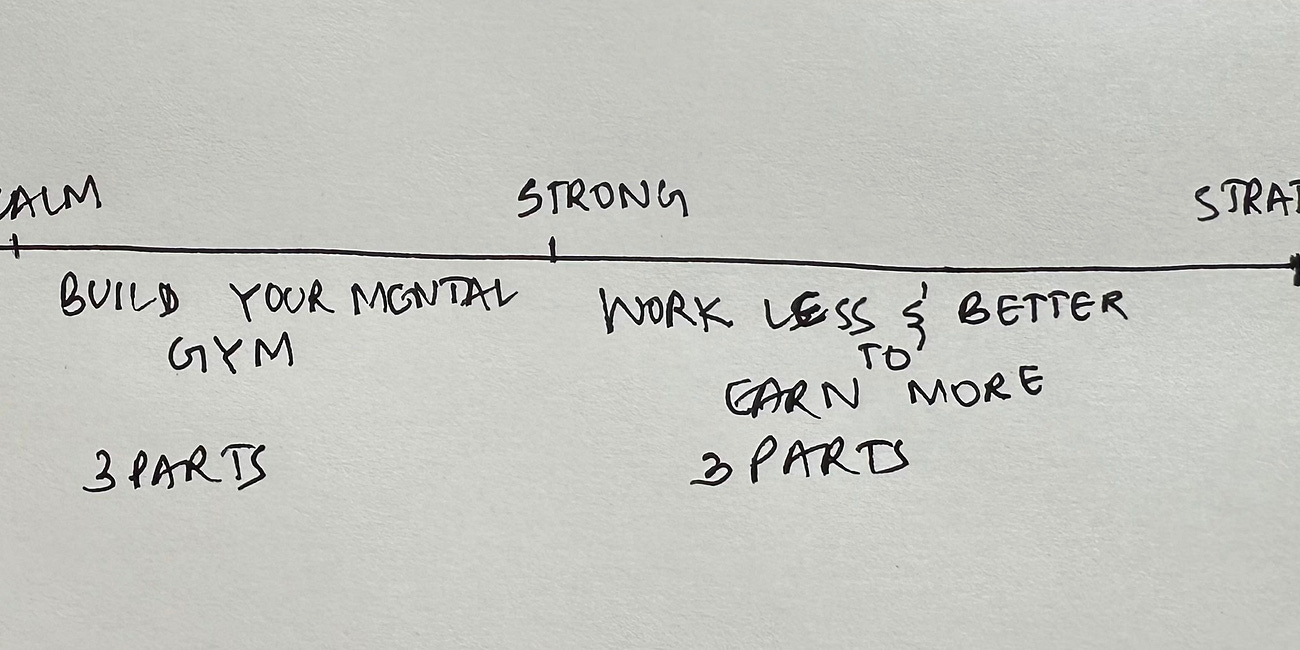
Section 1: Nervous System Regulation
Part 1 of 13: Wired But Tired? Start With Your Nervous System
Part 2 of 13: What Kind of Dysregulation Are You Experiencing?
Part 3 of 13: Holistic Regulation Protocol for Fight-or-Flight (For When Your System is Stuck in Overdrive) (this one)
Part 4 of 13: Holistic Regulation Protocol for Freeze (When You Feel Numb, Stuck, or Shut Down)
Part 5 of 13: Holistic Regulation Protocol for Overall Menstrual & Brain Health
Part 6 of 13: Understanding Your Type of Tired
Part 7 of 13: Restorative Protocols for the 7 Types of Unrest
Section 2: Build Your Mental Gym
Part 8 of 13: Neurotransmitters: The Gut-Brain Axis and Fuelling for Nervous System Regulation
Part 9 of 13: Neuroplasticity: The Vagus Nerve
Part 10 of 13: Neurogenesis: Interoception and Exposure to Hormetic Stress
Section 3: Work Less & Better to Earn More
Part 11 of 13: Peak Performance Training
Part 12 of 13: The Power of Creative Flow
Part 13 of 13: Productivity 101
Disclaimer: Understanding Research in Female Health and the Female Brain
The content provided in this series, "Build Your Mental Gym: A Brain Health Protocol for Women in Tech (in 13 parts)," is intended for educational purposes only and should not be construed as medical advice, diagnosis, or treatment. The information presented here is based on existing and available research in female health and the female brain, but it is essential to recognize that scientific understanding in these fields is continuously evolving.
1. Limited Scope of Information: The material covered in this series offers a general overview of topics related to nervous system regulation, with a focus on how it pertains to women in the field of technology. While efforts have been made to ensure the accuracy and relevance of the information presented, it is not exhaustive and may not encompass all aspects of female health or brain function.
2. Individual Variability: It is essential to recognize that individual experiences and health conditions may vary significantly. Factors such as genetics, lifestyle, medical history, and environmental influences can all impact an individual's nervous system regulation and overall well-being. Therefore, the information provided should not be applied universally without consideration of individual circumstances.
3. Consultation with Healthcare Professionals: Participants are encouraged to consult with qualified healthcare professionals or medical experts regarding any specific health concerns or questions they may have. While the content presented in this series may offer valuable insights, it is not a substitute for professional medical advice or personalised healthcare recommendations.
4. Evidence-Based Practices: Where applicable, the series content may reference evidence-based practices or findings from scientific research studies. However, it is important to recognise that research findings may be subject to interpretation, replication, or revision over time. Participants are encouraged to critically evaluate the evidence presented and consider the credibility and relevance of research sources.
5. Gendered Nature of Research: It is crucial to acknowledge the historical and ongoing gender biases present in scientific research, which have often resulted in a lack of comprehensive understanding of female-specific health issues and brain function. The underrepresentation of women in clinical trials and research studies has contributed to gaps in knowledge regarding the unique physiological and neurological characteristics of women. As such, participants should be aware that certain aspects of female health and brain function may not be fully understood or adequately researched.
6. Legal and Ethical Considerations: The creator of this series has made reasonable efforts to ensure that all content complies with applicable legal and ethical standards. However, the information provided should not be construed as medical advice.